Common Causes of Errors in Reconstituting Vaccines
Mistakes in reconstituting vaccines commonly happen for the following reasons:
- Vials have missing labels, making them impossible to identify correctly
- Incorrect usage of diluents
- Storing diluents for different vaccines in the same refrigerator without adequate labelling
In addition, Believing that vaccine diluents are interchangeable is a very common error. This is especially true with vaccines that require sterile normal saline or water. Often, due to either poor training or user error, healthcare workers can be led to believe that one vial of sterile water for injection is just as good as another. Thus, they reconstitute the vaccines with the first vial of sterile water available.
While this is an understandable mistake, it can lead to terrible results at the injection site for patients—especially for intramuscular injections or subcutaneous injections.
It is crucial to use only diluents recommended by the manufacturer to reconstitute vaccines. Especially for Single-dose vial vaccines—as if you mess up the diluent you lose the entire product.
Some common vaccines with specific diluent needs include:
- BCG vaccines
- Measles-containing vaccines
- Freeze-dried Haemophilus influenza type b (Hib) vaccines
- Yellow fever vaccines
How To Properly Handle Reconstituted Vaccines
1) Keep reconstituted vaccines cool and away from sunlight
The CDC recommends storing vaccines in a temperature range of 2oC to 8oC, and reconstituted vaccines are no different. Place them in slits made in a foam piece that sits in the top of the vaccine carrier. You keep the vaccine's temperature relatively constant and keep the vial out of direct sunlight.
2) Discard reconstituted vaccines after 6 hours
Vaccines like BCG, measles, yellow fever and freeze-dried Hib are preservative free. This means they do not have preservatives that limit the growth of microorganisms. Thus, they are susceptible to rapid microbial multiplication after reconstitution. The best way to combat this is to discard the reconstituted vaccine six hours after reconstitution.
3) Other Best Practices For Reconstituted Vaccines
Due to the sensitive nature of vaccines, it is best to wait until the person needing the vaccine injection is present. This is why some health care facilities have specific vaccination days and why it is recommended for people to arrive before reconstituting the vaccines.
- Reconstitute the vaccine only when the person needing the immunization is present
- Use a new syringe and needle to reconstitute each vaccine vial, and discard the syringe and needle after mixing.
Steps For Reconstituting Vaccines And Administering Them Safely

- Read and study the vial’s label
Product labels are full of information regarding any product, and vaccine diluent labels are no different. Specific information on the label includes the expiration date, vial size and manufacturer. You can compare these with the vaccine you want to reconstitute for best results(whether it is the diluent provided by that specific vaccine’s manufacturer.
- Cool the diluent to between 20C and 8oC before use to avoid heating the vaccine.
- Use a sterile syringe (with sterile syringe filters) and needle for mixing.
- Draw the entire contents of the diluent into the mixing syringe
- Empty the entire contents of the diluent into the vaccine vial
- Discard the used reconstituting syringe and needle
- Ensure that you do not leave the reconstituting needle in the vial, as this can leave the vial open to contamination
- Roll the vial between your fingers to mix the contents until all the vaccine powder has dissolved.
- Note the date and time you reconstituted the vaccine.
- Keep the reconstituted vaccine cool by placing it inside slits cut in the top of a foam pad.
It would be best to have a foam pad cut to fit a vaccine carrier, as WHO recommends this technique to keep the vaccine cold and protected from sunlight. The WHO recommendation is the best practice for keeping the vaccine cold, as any other technique, such as placing the vial in a cup of ice, can damage the vaccine or remove the vial label. - Discard all reconstituted vaccines at the end of the immunization session or six hours after reconstitution, whichever comes first, unless the product meets WHO criteria for use up to 28 days after opening, per the Multi-dose Vial Policy (2014).
- When administering the vaccine, withdraw it from the vial using a new needle and syringe and use the same to inject the vaccine. After giving the injection, drop the used syringe and needle into a safety box designated for this purpose without recapping.
- Use Vaccine Vial Monitors (VVM) as a visual trigger.
A VVM is a chemical-indicator label applied to a vaccine vial, ampoule, or another type of primary container by the vaccine manufacturer. You can find a VVM on nearly all vaccine vials supplied to national immunization programs procured through UNICEF. The VVM helps health workers to apply the multi-dose vial policy effectively to know when reconstituted vaccines should be discarded.
Other Ways to Avoid and Combat Vaccine Loss
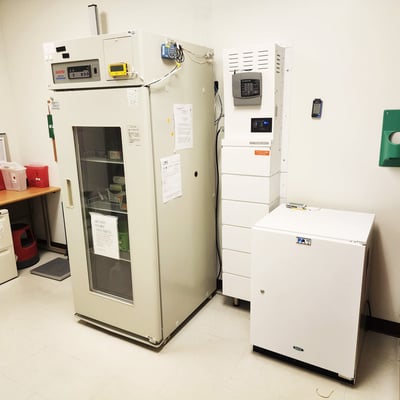
For end users of pharmaceuticals, the most likely scenario for them to experience a temperature excursion is because they’ve left the door open to a medical refrigerator/medical freezer or it has stopped running.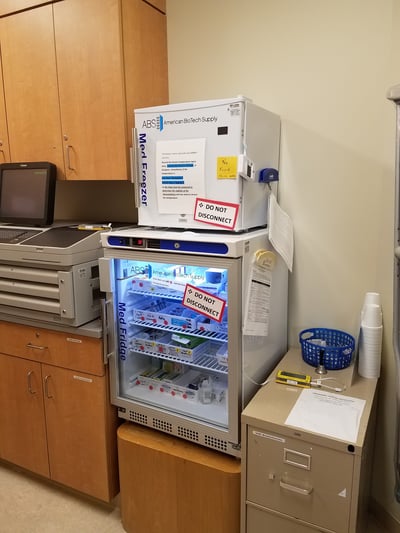
While door alarms and buffered temperature probes are fairly easy to source tools, a reliable and powerful backup power system for refrigerators can be harder to find.
Luckily, battery backup systems offer instant and automatic power for medical appliances as soon as the power goes out. As a result, no staff needs to be on-site to keep track of or start the generator and vaccines will continue to remain safe—with no extra work required.
Additionally, their vertical, cabinet-like design and leak-proof batteries mean they can be installed in even the tightest spaces and oriented in anyway to make them fit. Plus, if your medication or vaccine room is truly tight on space, a hardwired backup power unit can instantly supply remote power to your appliance—directly via the outlet its already plugged into.
Regardless of what kind of system is the best fit, they ensure that your entire stock of vaccines are protected from a sudden loss of power (and the resulting temperature excursions) by guaranteeing a seamless transition from utility power to backup power.
Even better, is that battery generators can be outfitted with as much power as you want. So system’s can be designed with enough power to protect a facility’s inventory:
- Overnight
- All day
- Over a weekend
- Or even for a whole week.
So, to protect your facility from tens of thousands of dollars in lost vaccine stock, speak to a Medi-Products battery backup expert.
They’ll help design you a system that both meets your power needs and will fit inside your facility—for a much lower cost than what your vaccines are worth. So a backup power system pays for itself the first time your power goes out.
Designing a custom system is as easy as taking a picture of your appliance’s nameplate, and a photo of the room where it’s in.
Then, you just email both photos to our Product experts, and we’ll provide you with multiple options for backup power protection.
For more information contact: 1.800.7653237